This is going to be just like getting your taxes done, right, except this  is going to go on year round and not just once a year. CMS has $54 million available to various entities to apply to become a “Navigator”. If you read it, there’s all types of groups that can apply for the federal funds. Maybe I should apply:) I could turn this blog into a “Navigator” blog. The grants are for “real people” and not algorithms this time so that’s a good thing as the exchanges will have plenty of those to navigate anyway. Here’s the short definition of a Navigator from CMS.
is going to go on year round and not just once a year. CMS has $54 million available to various entities to apply to become a “Navigator”. If you read it, there’s all types of groups that can apply for the federal funds. Maybe I should apply:) I could turn this blog into a “Navigator” blog. The grants are for “real people” and not algorithms this time so that’s a good thing as the exchanges will have plenty of those to navigate anyway. Here’s the short definition of a Navigator from CMS.
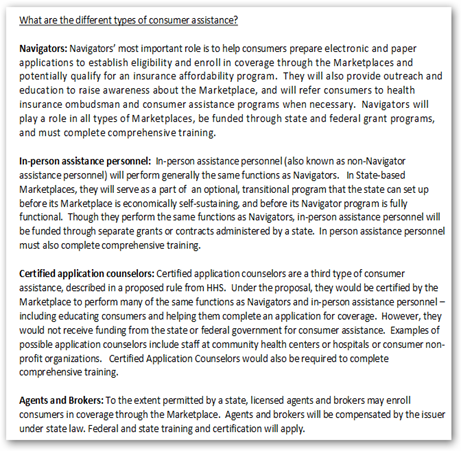
“Navigators' most important role is to help consumers prepare electronic and paper applications to establish eligibility and enroll in coverage through the Marketplaces and potentially qualify for an insurance affordability program. They will also provide outreach and education to raise awareness about the Marketplace, and will refer consumers to health insurance ombudsman and consumer assistance programs when necessary. Navigators will play a role in all types of Marketplaces, be funded through state and federal grant programs, and must complete comprehensive training”.
What I wonder about though is $54 million enough? I guess we will find out. This is not a pick choose business either…Here’s a few comments from the CMS page…
“Applicants that expect to assist a specific community or population may apply, although awardees must serve all consumers who seek their assistance. Smaller-sized entities and individuals are encouraged to partner with other entities or individuals to apply as a consortium”.
Successful applicants will be capable of conducting the following required Navigator duties:
- Maintain expertise in eligibility, enrollment, and program specifications;
- Conduct public education activities to raise awareness about the Exchange;
- Provide information and services in a fair, accurate, and impartial manner. Such information must acknowledge other health programs (such as Medicaid and the Children’s Health Insurance Program (CHIP));
- Facilitate selection of a Qualified Health Plan;
- Provide referrals to any applicable office of health insurance consumer assistance or health insurance ombudsman established under Section 2793 of the Public Health Service Act, or any other appropriate state agency or agencies, for any enrollee with a grievance, complaint, or question regarding their health plan, coverage, or a determination under such plan or coverage; and
- Provide information in a manner that is culturally and linguistically appropriate to the needs of the population being served by the Exchange, including individuals with limited English proficiency, and ensure accessibility and usability of Navigator tools, such as fact sheets, and functions for individuals with disabilities in accordance with the Americans with Disabilities Act and Section 504 of the Rehabilitation Act.”
In addition to Navigators, there are In person assistance people who will be available and certified application counselors…some of this makes my head spin just reading about the complex system of assistance created and we have not even arrived at the Exchange yet! You can thank your health insurance companies for this more than complex system to navigate. Doctors have had this mess for years and now it rolls over to consumers.
You will still be incredibly in the dark over many issues and basically getting insurance via an exchange has now been turned into a group effort it appears.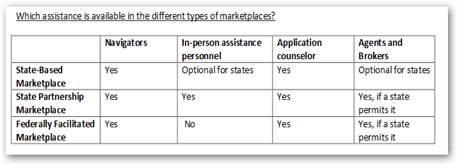
Now here’s how the people who will help you get trained….open the image and read it in your browser to see the small print and all of this information is available on a single pdf here.

Again when you get through all of this you can thank your for profit health insurance companies for all of it! I can say the complexities certainly gave CMS a lot of work to do and they probably need more in their budget for some of this at their end too. This is more like the “Affordable Complexity Act” if you ask me:) Maybe I should start using that terminology. At rate then once you have a policy purchased additional complexities arise too as insurers change their models all the time and have truckloads of analysts that work on their models and algorithms all the time. Whoops, this division not showing enough profit, well fix that business model and add some more complexity to make it work and it rolls downhill to the consumer to figure it out so keep those navigators busy.
If you listen to a former Wall Street Quant, she tells you that’s exactly what they do, she was told to fix the model and be a hero without seeing if the model is lying either accidentally or on purpose as she saw in one of her jobs first hand how people lie with risk models. So be assured that as soon as you feel settled in for a few moments everything could change again as soon as the insurers add some more complexities to make their models work. They all do it just as the banks do. As I said today on another blog post, banks and insurers are just pretty much software companies anymore, working models and algorithms.
Banks Are Actually Just Software Companies and the Same Can Pretty Much Be Said for Health Insurance Companies As Well-5 Unspoken Reasons Tech Projects Fail
Don’t forget the user fee that will probably be passed on to you that was approved by the government.
Insurance Exchanges Now to Have a User Fee for Insurers to Pay But It Gets Charged Back to the Consumer
So we are getting prepared for the big date in October when all this IT Infrastructure and work comes together so you can have health insurance…and if enough flawed data is worked “out” of the systems so it will be useable.
Health Insurance Exchanges–Will State IT Departments Be Able to Meet the Deadlines…A Wait and See, And What About That Flawed Data?
Last week we saw this sane battle between CMS and the Inspector General with the Inspector General requesting that on the Medicare Insurance site that CEOs of insurance companies certify the information they supply….it shows the huge level of frustration I think with all of this coming together. Stay tuned for the next news in the complex complicated world of health insurance..or just give it up and go to Wal-Mart as they want to be an exchange too:) BD
CMS and the Inspector General with the Inspector General requesting that on the Medicare Insurance site that CEOs of insurance companies certify the information they supply….it shows the huge level of frustration I think with all of this coming together. Stay tuned for the next news in the complex complicated world of health insurance..or just give it up and go to Wal-Mart as they want to be an exchange too:) BD
CMS and Inspector General Duking It Out Over Government Website Data That Helps Consumers Find Health Plans- Just Wait Until the Exchanges Get Going And We Find Those Shortcomings…
The Obama administration has set aside $54 million in federal grants to fund the first year of Obamacare "navigators," the community activists, union members and health professionals who will be paid to help an estimated 7 million Americans sign up for health exchanges nationwide.
The Centers for Medicare & Medicaid Services, which will run Obamacare, said that those seeking grants must apply by June 7. The health care program kicks in Oct. 1, when Americans can sign up for health care coverage to begin Jan, 1.
"Navigators will be an important resource for the millions of Americans who are eligible to enroll in new coverage opportunities through the Marketplace starting in October of 2013," acting Medicare administrator Marilyn Tavenner said in a statement.
No comments:
Post a Comment